Nasima Begum is all too aware of the risks of childbirth in Bangladesh. At only 18, she has already lost two babies.
"The first one died because we didn't know that the mother needed medical check-ups during pregnancy. The second one died because we took Nasima to a private clinic where there were no trained birth attendants," her husband, Selim Reza, 25, a rickshaw driver, told IRIN.
"This time we were careful. I took her to a locally trained birth attendant every three months during her pregnancy and she had a safe birth," he said.
According to the UN Children's Agency (UNICEF) State of the World's Children Report 2008, Bangladesh has the worst maternal mortality rate (MMR) in South Asia at 570 per 100,000 live births.
In comparison, the rates in neighbouring India and Pakistan are 450 and 320 respectively, the report states.
According to Bangladesh's 2007 Demographic and Health Survey, 21,000 mothers die annually of pregnancy and childbirth-related causes, principally because skilled birth attendants account for just 13 percent of all deliveries in Bangladesh, according to government health experts.
The problem is particularly pronounced in rural areas, where more than 75 percent of the country's 150 million inhabitants live.
"Eighty percent of maternal deaths happen in the countryside," said Sabera Khatun of the department of gynaecology and obstetrics at the Bangabandhu Sheikh Mujib Medical University in Dhaka. "Medical facilities have not reached the rural areas as extensively as they should."
Major causes
Most women die of haemorrhaging, followed by anaemia, hypertensive disorders, obstructed labour and abortion, explained Ferdousi Begum of the Dhaka Medical College Hospital.
CARE Bangladesh, which has been organising community initiatives to promote maternal and neo-natal health for past 25 years, cites delays in seeking medical assistance and receiving the appropriate healthcare, as well as transportation problems, as contributing factors.
Findings from the 2007 Demographic and Health Survey concluded that just over half of all pregnant women received any institutional health services during childbirth, while significantly fewer received institutional post-natal healthcare.
"Fifty-six percent of women go to hospitals and clinics for ante-natal care, but the rate is only 18 percent for post-natal care," said Laila Anjumand Banu, health and environment secretary of Bangladesh Mahila Parishad (BMP), a prominent women's rights organisation.
More resources required
Abul Barakat of the Bangladesh Economic Association blames the high maternal mortality rate on poor budgetary allocation by the government.
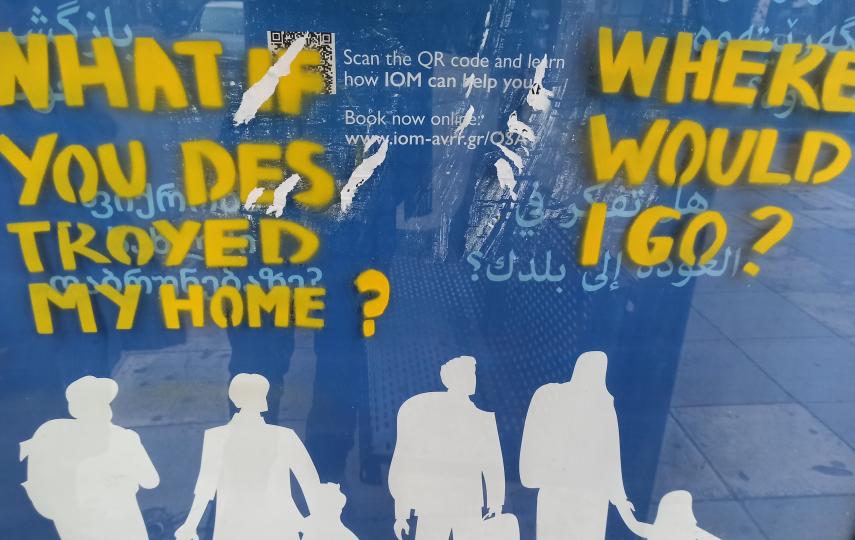
 Photo: Shamsuddin Ahmed/IRIN  |
| Bangladesh needs an additional 10,000 midwives |
"Safe delivery services make up only 9.5 percent of the health budget," Barakat explained.
"A two to three times increase in budget is required for delivery care components," he said, adding that the number of service providers in emergency obstetric care, particularly doctors and nurses, should be increased.
However, Bangladesh's per capita health expenditure is just US$4.62, while only 1 percent of gross domestic product goes on health, he said. In addition, coverage is limited. Since 1998, a comprehensive maternal healthcare project has been introduced to only 80 of the country's 482 sub-districts.
Shortage of midwives
To reduce maternal and infant mortality, according to the Bangladesh Nursing Council, the country needed another 10,000 midwives to boost the 22,000 employed at present.
Moreover, a six-month extended training was required to allow them to work as full-time midwives, stated a recent paper by the Nursing Council.
At present, nurses are only given midwifery training in the last year of their four-year nursing course.
"But these nurses cannot provide their full services to provide special care to mothers and newborns because nurses have to attend to various official and clinical responsibilities that are not related to pregnancy and childbirth," noted Begum Shamsun Nahar, registrar of the Bangladesh Nursing Council.
"Midwives can play an important role in reducing maternal and infant mortality by ensuring proper services during pregnancy and the delivery period and through ante-natal care," she said.
To fulfil the Millennium Development Goal of improving maternal health, Bangladesh will need to increase the presence of skilled birth attendants to 50 percent of births and bring down the MMR to 240 by 2015.
sa/ds/mw
This article was produced by IRIN News while it was part of the United Nations Office for the Coordination of Humanitarian Affairs. Please send queries on copyright or liability to the UN. For more information: https://shop.un.org/rights-permissions